ICU Management & Practice, Volume 24 - Issue 3, 2024
An analysis of technical alarms to guide hospital-based alarm management strategies and inform monitoring manufacturers on needed improvements to technical alarm algorithms used in bedside ECG monitors.
Introduction
Hospital-based electrocardiographic (ECG) monitors are configured to alarm for a number of different types of arrhythmias, ST-segment changes, and QT interval lengths that are designed to alert busy nurses. However, accurate detection of ECG abnormalities/features requires a clean signal. Most ECG devices include technical and/or inoperative alarm algorithms that are designed to notify and inform the nurse when a specific signal quality issue arises to minimise monitoring interruptions. For example, one type of technical alarm is ECG lead off (single or multiple), or ECG leads fail (no signal) that informs the nurse to replace either the skin-electrode(s) and/or the lead wire(s). Technical alarms can be configured to either generate an alarm sound (e.g., warning, continuous foghorn tone) or as an inaudible text message alert that flashes on the bedside monitoring screen. While there are no established guidelines for optimal alarm settings, technical alarms for artefact (noisy signal) or when a single ECG lead is off are typically configured as inaudible text message alerts (flash text on the bedside monitor); thus, they do not need to be silenced by the nurse. In general, inaudible text is selected for these types of alarms because there is still an ECG signal present; thus, arrhythmia detection is maintained. Many hospitals choose to configure some more important technical alarm types using an audible alarm configuration to ensure that a clean ECG signal is established promptly. For instance, when more than one ECG lead is off, or there is an extended period of time in a technical alarm condition (sustained artefact), an audible alarm is used since both of these types of technical issues may turn off or suspend arrhythmia detection software and an arrhythmia could be missed.
While technical alarms (i.e., artefact, ECG lead(s) fail, ECG lead(s) off) are designed to ensure optimal ECG signal quality for arrhythmia detection, these types of alarms are extremely common and can contribute to alarm fatigue in nurses. In a comprehensive one-month ECG alarm study in 461 intensive care unit (ICU) patients of the more than 2.5 million total alarms generated, 32% (791,632) were technical alarms (Drew et al. 2014). Alarm fatigue associated with bedside ECG and physiologic (vitals sign) monitors can create the following unsafe situations in patient care: (1) inadvertently ignoring alarms due to desensitisation (i.e., alarm noise is assimilated into a nurses’ workflow); (2) lowering the volume of alarms to reduce patient and family stress from alarm noise; (3) completely silencing alarms; and/or (4) delayed response to alarms (Bonafide and et al. 2015). Additionally, nurses often experience overload in various forms during their work (e.g., cognitive and physical), which is further compounded by ECG device-related alarm fatigue (Lewandowska et al. 2020).
Alarm fatigue and the related responses set the stage for a major patient safety issue, which has devastating effects on both nurses and patients. Alarm fatigue has been associated with over 650 hospital deaths (Dee et al. 2022; Ruskin and Hueske-Kraus 2015), and in a retrospective study from 2011, there were 216 patient deaths linked to issues with alarm fatigue (Shue and Ortiz 2019). Importantly, these data are dated, and because few substantive interventions have been introduced to solve alarm fatigue, morbidity and mortality are likely much higher.
There have been several hospital-based studies that have evaluated technical alarms generated from ECG monitors (Albert et al. 2015; Cvach et al. 2013; Drew et al. 2014; Graham and Cvach 2010; Sendelbach et al. 2015; Shue and Ortiz 2019; Watanakeeree et al. 2021). One observational study conducted in adult ICU patients showed that 32% (791,632) of more than 2.5 million total alarms were technical alarms, and the vast majority (358,277) were for artefact followed by single ECG lead fail (90,547) (Drew et al. 2014). Technical alarms for arrhythmia suspend and ECG leads off (no signal) were not reported. In a subsequent secondary data analysis from this study, artefact, ECG leads off/fail, and arrhythmia suspend were reported in ICU patients with a left ventricular assist device (Watanakeeree et al. 2021). Artefact was the most common technical alarm (96%) followed by ECG leads fail (3.5%) and then arrhythmia suspend (0.5%). Of the remaining studies, technical alarms were examined at pre- and post-quality improvement (QI) project implementation (Cvach et al. 2013; Graham and Cvach 2010; Sendelbach et al. 2015; Shue and Ortiz 2019), and one examined alarm rates when using disposable versus non-disposable ECG lead wires (Albert et al. 2015). Two studies examined both artefact and ECG leads off/fail alarms (Albert et al. 2015; Sendelbach et al. 2015), two examined both ECG leads off and arrhythmia suspend (Cvach et al. 2013; Graham and Cvach 2010), and one examined only ECG leads off (Shue and Ortiz 2019). To our knowledge, no study has examined specific technical alarm types in a comprehensive manner (i.e., types, duration, possible patient/clinical factors). A more extensive analysis of technical alarms for these characteristics may help guide hospital-based alarm management strategies and inform monitoring manufacturers on needed improvements to technical alarm algorithms used in bedside ECG monitors.
Purpose
The purpose of this study was twofold: (1) examine the number, type, and duration of technical alarms for artefact; arrhythmia suspend, and ECG leads fail, and (2) examine whether demographic (age, sex, race) factors, clinical features (body mass index, impaired cognitive status, tremor, smoking), mechanical ventilation and/or ICU type (cardiac, medical/surgical, or neurological,) are associated with technical alarms.
Methods
Study Design
This was a secondary data analysis using data from a comprehensive one-month alarm study among a consecutive cohort of adult intensive care unit patients (Drew et al. 2014). The occurrence rate, type, and clinical features hypothesised to increase the occurrence of technical alarms (described below) for the artefact, arrhythmia suspend, and ECG leads fail were examined for this analysis. The Institutional Review Board (IRB) approved the study (IRB# 12-09723) with a waiver of patient consent because the alarm data was captured in the background, did not interrupt patient care, and was analysed retrospectively.
Sample and Setting
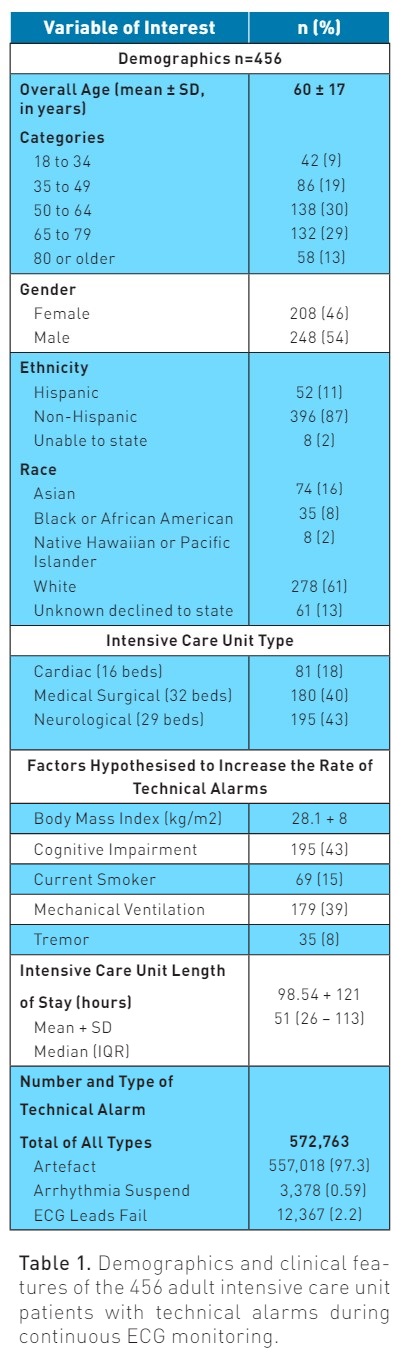
The primary study included 461 consecutive adult ICU patients with continuous ECG monitoring from three types of ICUs, including cardiac (16 beds), medical/surgical (32 beds), and neurological (29 beds), at a large tertiary-quaternary medical centre over a 31-day period. For this study, based on our prior work (Bawua et al. 2022; Drew et al. 2014; Harris et al. 2017; Suba et al. 2019), we hypothesised that BMI, being a current smoker, having cognitive impairment, a tremor, or mechanical ventilation would be associated with a higher rate of technical alarms. There were five patients (1.08%) who did not have BMI documented and were subsequently excluded, leaving 456 ICU patients available for analysis. Demographics, including sex, age, race, and ethnicity, were obtained from the electronic health record (EHR). Additionally, ICU type (cardiac, medical/surgical and neurological) and the use of mechanical ventilation were acquired from the EHR.
Alarm Data Capture System
Our data capture system has been described in detail previously (Drew et al. 2014; Pelter et al. 2023). Briefly, all ECG and physiologic monitor waveforms (i.e., seven ECG channels [I, II, III, aVR, aVL, and aVF], arterial blood pressure, pulse oximetry [Sp02], impedance respirations), numeric vital signs, and alarm types (both audible and inaudible) were acquired via a secure data capture system. Data were downloaded to a secure research server approved by our hospital and were extracted into Extensible Markup Language (XML) files for analysis.
Technical Alarm Types
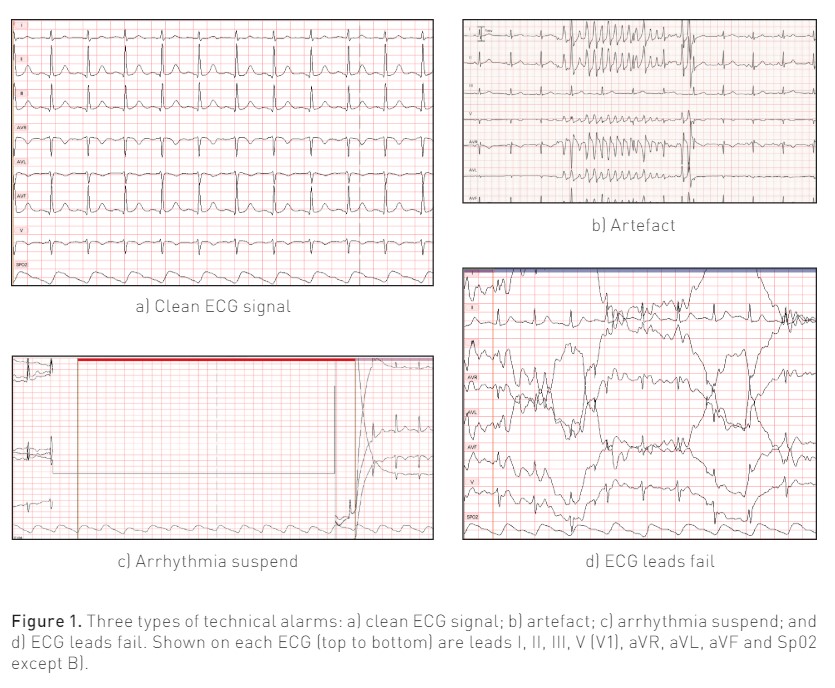
Technical alarm types, called system status alarms by the vendor, we examined included: (1) artefact (noisy signal); (2) arrhythmia suspend (no arrhythmia detection [software off] due to sustained artefact >20 seconds in the prior 30 seconds); and (3) ECG leads fail (no discernible ECG waveform displayed). Figure 1 shows the type of technical alarms examined, as well as a clean signal ECG. Technical alarms greater than 20 minutes in duration were excluded as we assumed that this likely indicated that the patient was not being monitored (e.g., procedure on/off unit, bathing, etc.), but the monitor had not been paused. Alarms for artefact were configured in the bedside monitor as an inaudible text message alert. In this alarm condition, full arrhythmia processing is suspended while the lethal arrhythmia algorithm is still active. However, its accuracy may be hindered by the artefact. Alarms for arrhythmia suspend and ECG leads (plural) fail were configured as an audible warning alarm. In these alarm conditions, a repeating foghorn tone sounds, and arrhythmia analysis is suspended until the technical alarm condition is resolved.
Data Analysis
Descriptive statistics were used to describe sample demographics, factors hypothesised to increase the rate of technical alarms, ICU type, length of ICU stay (hours), and frequency and duration of each technical alarm. Descriptive statistics are reported as frequencies for categorical variables and mean ± standard deviation (SD) for continuous variables. Data were tabulated in the overall sample and grouped based on the type of technical alarm. For the statistical analysis, we used medians and interquartile ranges (IQRs) due to the high variability in the number of technical alarms a patient may have generated. For this analysis, IQRs were weighted (weighted median, weighted 25th percentile, weighted 75th percentile) by ICU monitoring time. A negative binomial GLM regression model was used to evaluate both univariate and multivariate associations because of the variability of alarm counts per patient. A p-value of <0.05 was used as the critical value to determine statistical significance. All statistical analyses were conducted using R (v4.3.2; R Core Team 2023).
As mentioned above, due to high variability in the number of all technical alarm types (i.e., one patient could have one while another patient could have hundreds), we used the following approach: (1) occurrence rates for each alarm type were calculated per 10 hours of monitoring; (2) median and 25th and 75th percentiles of the distribution were weighted by monitoring time, and; (3) a chi-square test was used to test for deviance of the binomial GLM, where a p-value of <0.05 was used to determine statistical significance. Predictors in the multivariate model were included based on subject-matter knowledge and the conceptual model. For this study, based on our prior work (Drew and Harris et al., 2014; Bawua and Miaskowski et al., 2022; Suba and Sandoval et al.,2019), we hypothesised that BMI, being a current smoker, having cognitive impairment, a tremor, or mechanical ventilation would be associated with a higher rate of technical alarms; hence, only patients with these variables documented were examined.
Results
Entire Sample
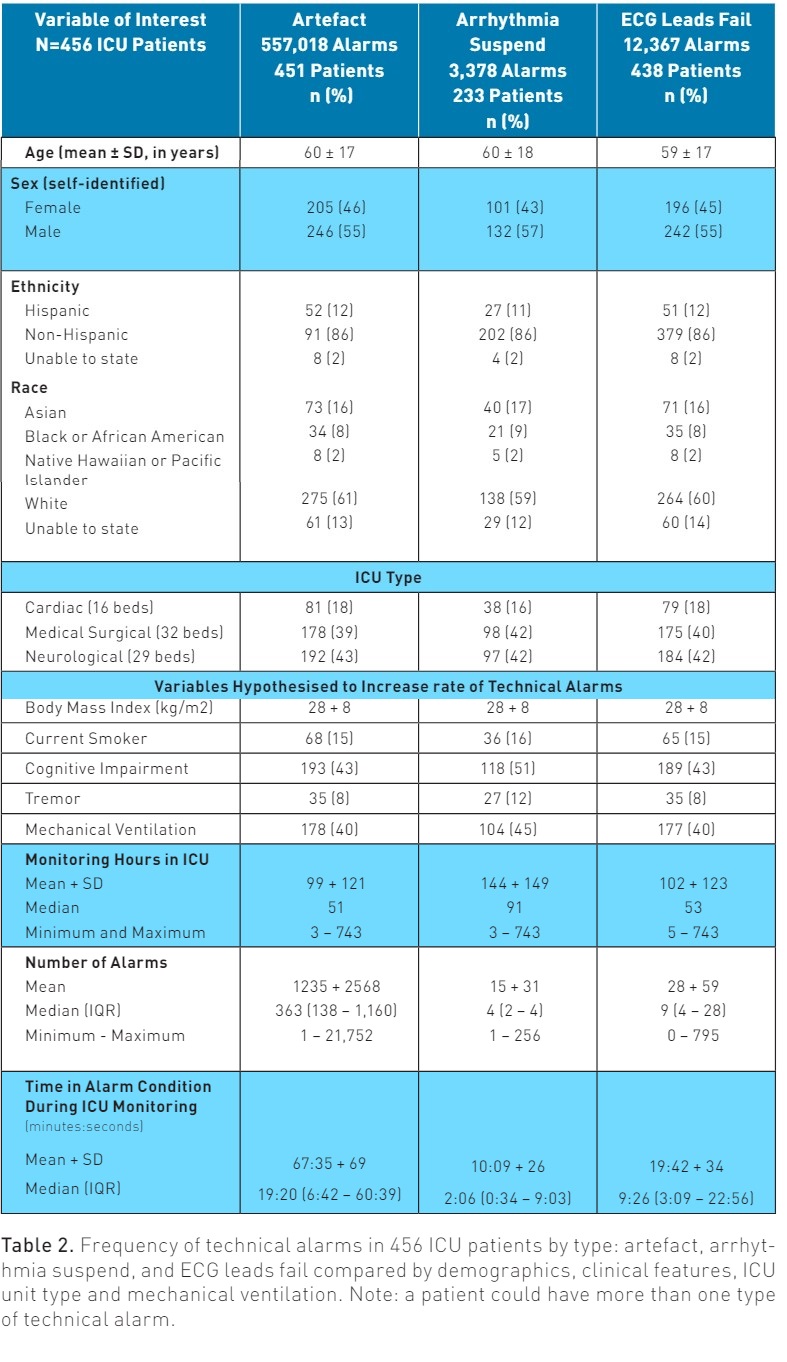
Table 1 shows the 456 adult ICU patients included in the study. The total number of technical alarms was 572,763. Of the total, 557,018 (97%) were artefact alarms, 3,378 (0.6%) were arrhythmia suspend alarms, and 12,367 (2.2%) were ECG leads fail.
Patient Characteristics by Alarm Type
Each technical alarm type was compared by patient demographics, ICU type, clinical features, and mechanical ventilation as illustrated in Table 2. All but 5 (n=451, 99%) patients generated one or more artefact alarms, 233 (51%) arrhythmia suspend alarms and 438 (96%) ECG leads fail alarms. It’s important to note that a single patient could have more than one type of technical alarm. Patients in either the medical surgical or neurological ICUs had the highest proportion of alarms as compared to the cardiac ICU, which again likely reflects the number of beds in each unit.
The proportion of the three technical alarm types compared by, age, sex, ethnicity, race, ICU type, BMI, current smoker, cognitive impairment, tremor, and mechanical ventilation were equivalent (Table 2). Due to high variability in the number of technical alarms, the median values are discussed here and were used in the statistical analysis described below. Median ICU monitoring hours was longest in the patients with arrhythmia suspend alarms (91 hours), followed by ECG leads fail (53 hours), then artefact (51 hours). The highest median number of alarms was for artefact (363), followed by ECG lead fail (9), then arrhythmia suspend (4). The median time in an alarm condition was highest for artefact (19:20 min:sec), followed by ECG leads fail (9:26 min:sec), then arrhythmia suspend (2:06 min:sec).
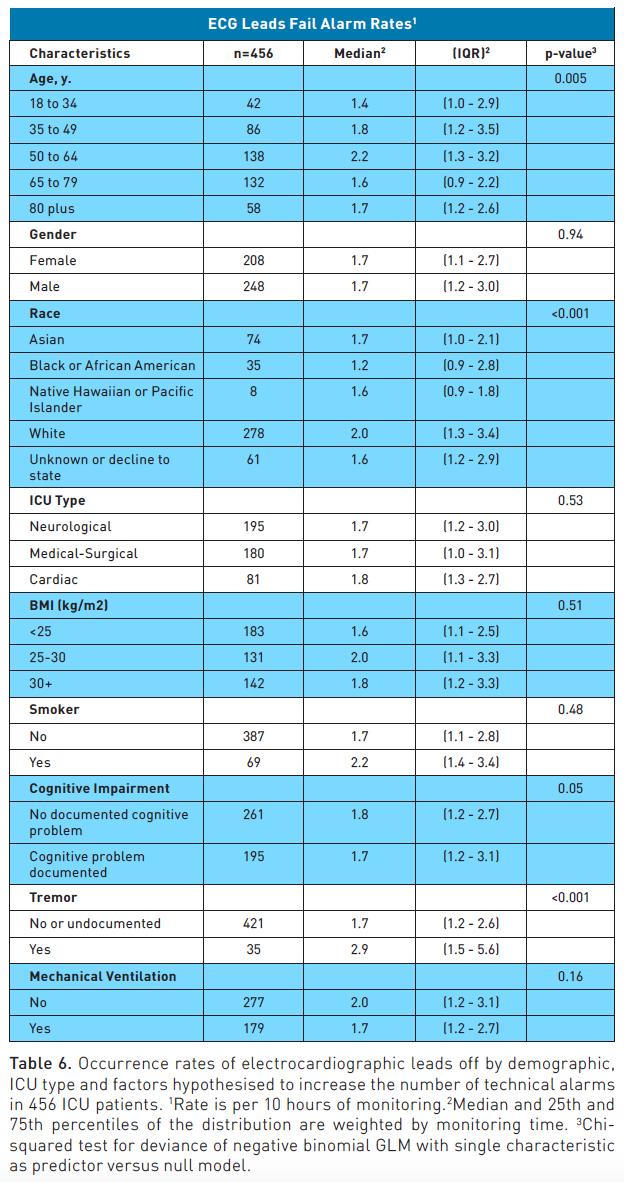
Duration of Technical Alarms
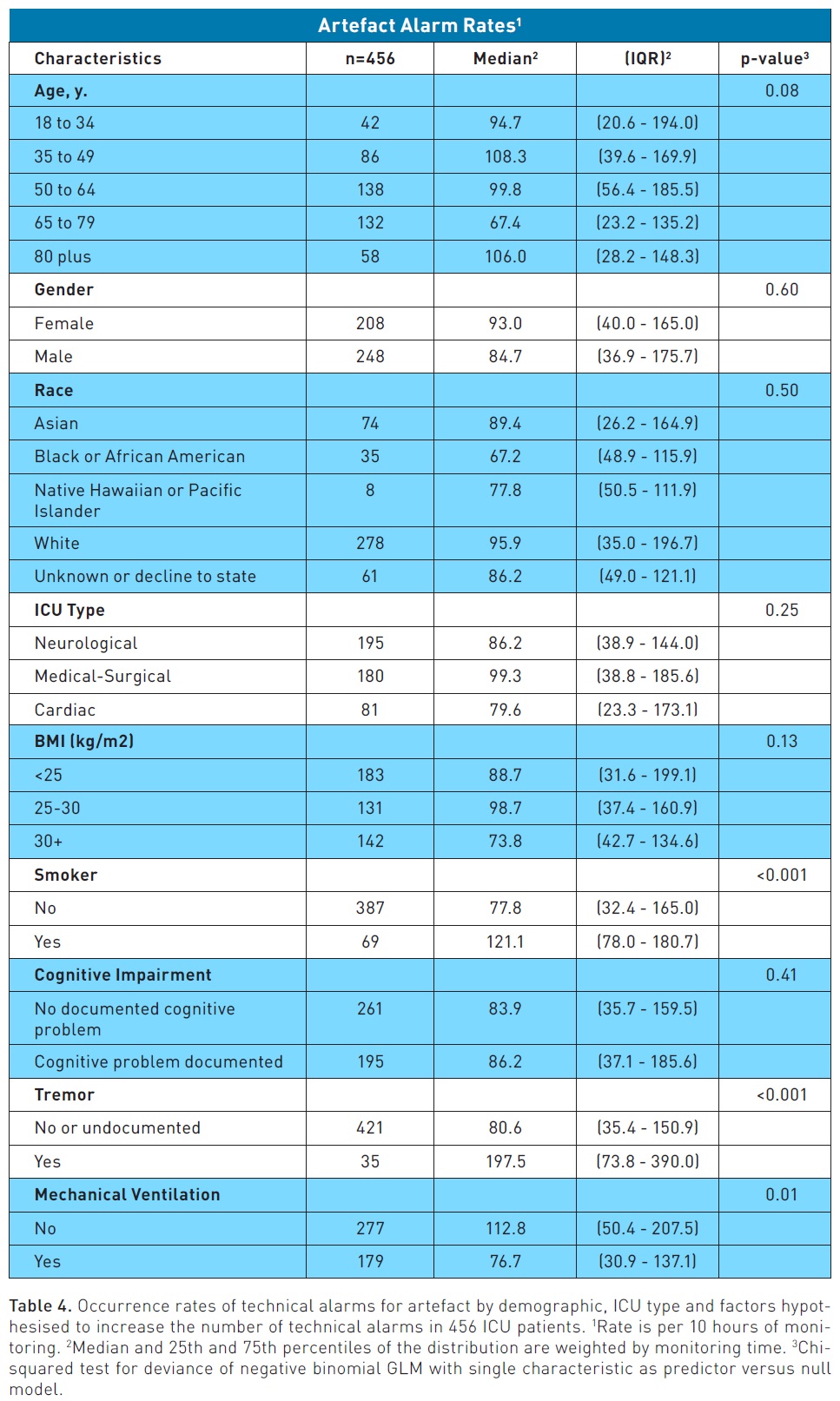
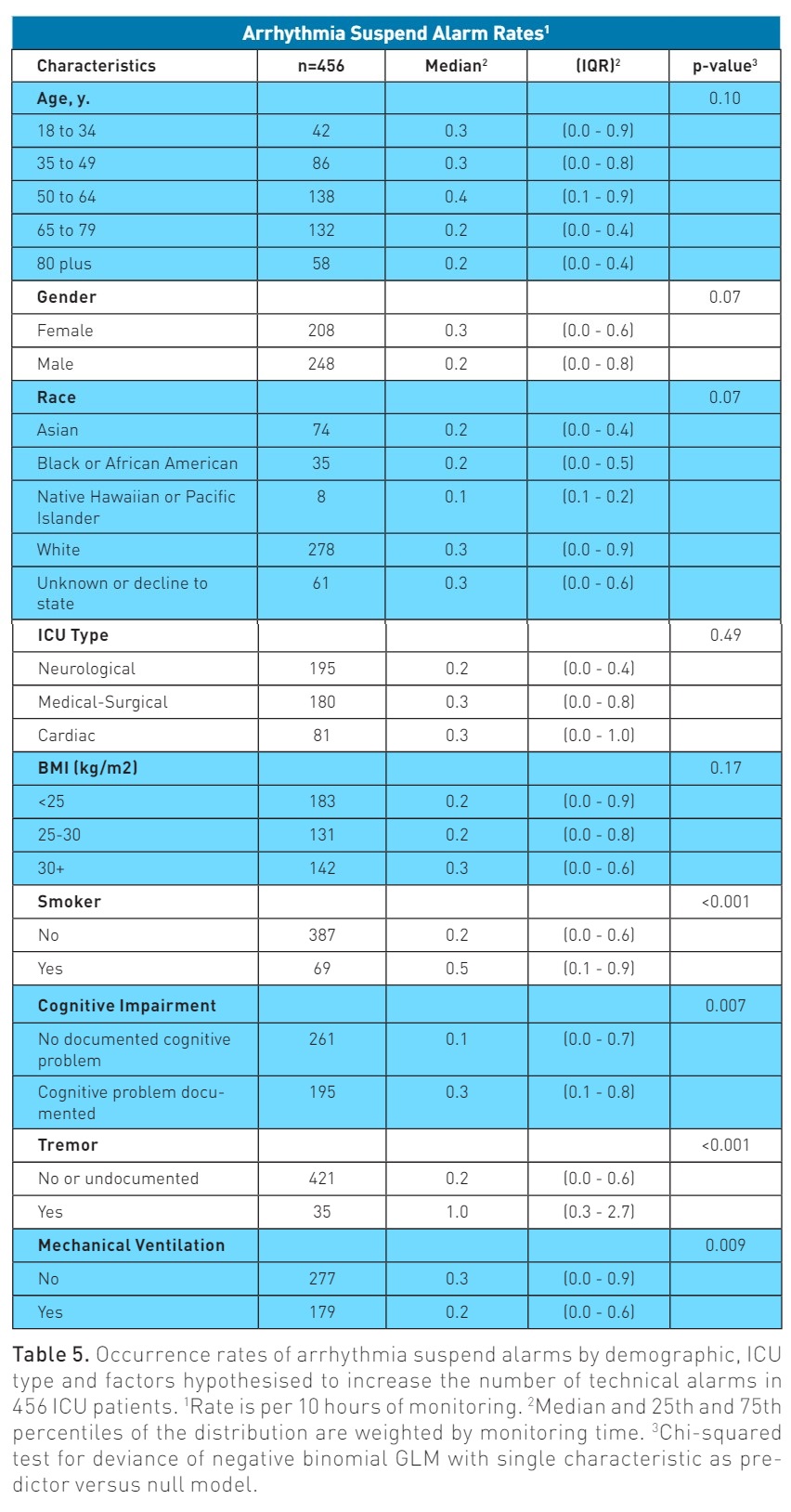
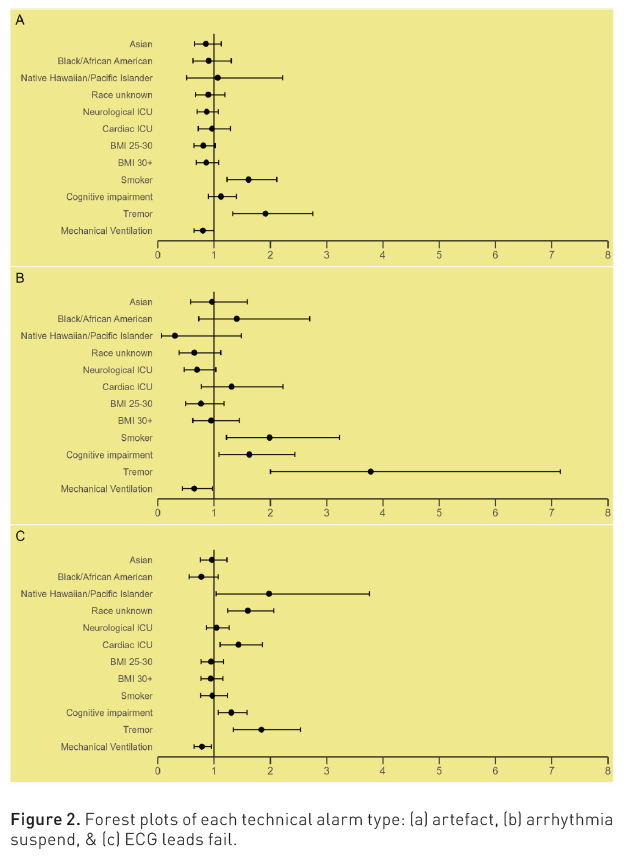
Most of the technical alarms were two seconds in length, specifically, 58% (n=323,070) of the artefact alarms, 60.5% (n=2,044) of arrhythmia suspend alarms and 64% (n=7,915). Each type of technical alarm was categorised into duration time frames using the following categories, which could help guide alarm configuration delays and/or algorithm development: two seconds to Below we describe the univariate and multivariate analysis for each technical alarm type. Artefact: In the univariate analysis, being a current smoker and having a tremor was associated with higher rates of artefact alarms. Being treated with mechanical ventilation was associated with fewer alarms (Table 4). Figure 2 shows a forest plot of the multivariate analysis. Being a current smoker and having a tremor remained significant predictors of artefact alarms. Patients treated with mechanical ventilation were less likely to have artefact alarms. All of the other variables included were not significant. Arrhythmia Suspend: In the univariate analysis, being a current smoker, having cognitive impairment and having a tremor was associated with higher rates of arrhythmia suspend alarms. Being treated with mechanical ventilation was associated with fewer alarms (Table 5). Figure 2 shows a forest plot of the multivariate analysis. Being a current smoker, having cognitive impairment and having a tremor remained significant predictors of arrhythmia suspend alarms. Being treated with mechanical ventilation was associated with fewer alarms. All of the other variables included were not significant. ECG Leads Fail: In the univariate analysis, age, race and having a tremor were associated with higher rates of ECG leads fail alarms. Being a current smoker, having cognitive impairment, and treatment with mechanical ventilation were not significant (Table 6). Figure 2 shows a forest plot of the multivariate analysis. The race category of Native Hawaiian/Pacific Islander and unknown race (patient unable to state due to acute illness) were significant predictors of ECG lead fails alarms, but the sample was small. In addition, being treated in the cardiac ICU, having cognitive impairment, and having a tremor remained significant predictors of ECG leads fail alarms. Being treated with mechanical ventilation was associated with fewer alarms. All of the other variables included were not significant. To our knowledge, this is the first study to examine factors associated with three types of technical alarms, specifically artefact, arrhythmia suspend, and ECG leads fail, in 456 consecutive ICU patients. Artefact represented the vast majority of alarms, 97%, followed by ECG leads fail, 2.2%, then arrhythmia suspend, 0.5%. Fifty-eight percent of artefact alarms and more than 60% of arrhythmia suspend, and ECG leads fail alarms were two seconds in duration. Patients who were current smokers at admission were more likely to have artefact (1.16 times more likely) and arrhythmia suspend (1.98 times more likely) alarms. Having a tremor was associated with all three types of technical alarms (1.91 times more likely for artefact; 3.78 times more likely for arrhythmia suspend; and 1.84 times more likely for ECG leads fail). Documented cognitive impairment was associated with arrhythmia suspend (1.63 times more likely) and ECG leads fail alarms (1.30 times more likely). Being treated with mechanical ventilation was associated with fewer alarms for all three types of technical alarms. Of seven prior published studies that we identified as relevant to compare with our study, artefact was reported in four (Albert et al. 2015; Drew et al. 2014; Watanakeeree et al. 2021). Two were associated with this secondary data analysis and report the same findings as out study (e.g., the artefact was the most common type). Of the two remaining studies, one did not report specifically on artefact alarms but rather grouped artefacts with other types of alarms (Sendelbach et al. 2015). However, Albert et al. (2015) did report on artefact alarms. In their study, artefact alarm rates were examined by ECG lead wire type (disposable versus reusable) in 1,611 unique cardiac telemetry unit patients with 2,330 admissions. They found that artefact alarms were the second most common type of technical alarm (ECG leads off/fail most common), which is different than our study, where we found the artefact was by far the most common alarm. Their study included cardiac telemetry unit patients, whereas ours included ICU patients. This may suggest that cardiac telemetry unit patients are more susceptible to leads off/fail, which is not entirely surprising given that these patients are more mobile than ICU patients who are mostly in bed. It is worth noting that in their study, the rate of artefact versus ECG leads off/fail was similar (2,993 artefact versus 3,555), suggesting that both types are common. Their study is interesting in that it showed that there were fewer artefact alarms in patients who had disposable ECG lead wires that were designed with a patented push-button feature. This study sheds light on one possible solution to reducing artefact alarms. None of the studies examined patient-level factors associated with artefact alarms; hence, our study offers new information. We found that patients who were current smokers at admission or had tremors were more likely to have artefact alarms. Our study shows that patients with these characteristics may need more focused alarm management strategies and/or treatment(s). For example, the effects of nicotine withdrawal may need to be treated. Determining whether a tremor is part of the patient’s history could be useful, or if new, it may suggest untoward effects of medications (i.e., drug induced Parkinson’s) (Jeong et al. 2021; Shin and Chung 2012) Interestingly, being treated with mechanical ventilation was protective against artefact alarms. This is in contrast to prior studies our group has published showing that mechanical ventilation was associated with false arrhythmia and respiratory rate type alarms (Bawua et al. 2022; Harris et al. 2017). Sedation during mechanical ventilation may be one explanation, but this finding needs further investigation. Of seven prior published studies that we identified as relevant to compare with our study, arrhythmia suspend was reported in three (Cvach et al. 2013; Graham and Cvach 2010; Watanakeeree et al. 2021). One was a secondary data analysis using our dataset that included only three patients with a left ventricular assist device. Arrhythmia suspend was the least common type, as was found in our study. In a study by Cvach et al. (2013) arrhythmia suspend alarms were examined in a pre-and post-QI study assessing whether daily skin electrode changes reduced these types of alarms. The investigators showed that this type of alarm decreased by 60% in the medical progressive care unit and 74% in the cardiology care unit following the intervention. This suggests that daily skin electrode changes may reduce this type of alarm. However, patient and/or clinical characteristics associated with this type of alarm were not reported. In a study by Graham et al. (2010), arrhythmia suspend alarms were examined pre- and post-QI implementation focused on several initiatives (i.e., changing default settings, education on individualising patient default settings, adjusting audible alarms, and a software modification) in the progressive care unit. Prior to the intervention, there were 634 arrhythmia suspend alarms, and after the intervention, they increased to 1,116. It is unclear why there were more of these types of alarms post-QI implementation, but overall alarm rates for a multitude of other alarm types were reduced post-QI implementation. One intervention used by the investigators was to adjust alarm settings (e.g., warning [foghorn tone] to an inaudible message) to reduce nuisance alarms (true but not actionable). However, it was not described whether arrhythmia suspend was adjusted in their study from a warning alarm to an inaudible message alert. If this adjustment was made, this might explain why there were more arrhythmia suspend alarms post-intervention. For example, if an alarm tone was not generated, the nurse would be less likely to solve this issue because it was set as an inaudible message alert. This type of technical alarm is generated when certain conditions are present, such as ECG leads off or, in the case of the monitor in place during this study, sustaining artefact>20 seconds in the prior 30 seconds. This indicates that arrhythmia analysis has been suspended (off), which has important clinical implications as an arrhythmia might be missed. In our study, only 0.6% of the patients had this type of alarm, and the mean and median time a patient was in this alarm condition was 10 minutes and 2 minutes, respectively. We found that patients who were current smokers at admission and those with cognitive impairment or tremors were more likely to have this type of technical alarm. Therefore, nurses should assess for these patient characteristics and, if indicated, consult with the care team on strategies to minimise the effects of these clinical features (i.e., nicotine withdrawal treatment) if possible. These types of patients may also benefit from daily skin electrode changes, which have been shown to reduce artefacts that can create this type of alarm (Cvach et al. 2013; Sendelbach et al. 2015). Contrary to artefact and arrhythmia suspend, all seven prior published studies that were relevant to compare to our study had measured ECG leads fail alarms (Albert et al. 2015; Cvach et al. 2013; Drew et al. 2014; Graham and Cvach 2010; Harris et al. 2017; Shue and Ortiz 2019; Watanakeeree et al. 2021). In the studies by Shue and Ortiz (2019) and Sendelbach et al. (2015), ECG leads fail alarms were measured, but grouped together with other types of technical alarms (e.g., no signal or telemetry battery low) or measured per day as a mean number of all ECG alarms. These two studies implemented several tests of change but it’s not clear how these interventions specifically affected ECG leads fail alarm rates. Our study was designed to measure the occurrence rate of ECG leads fail alarms, which was found to be 2.2% (12,367) of all of the technical alarms. This type of data could be helpful in determining whether a reduction in ECG lead fail/off alarms are due to various interventions proposed in previous studies. Two QI implementation projects had a specific focus on ECG leads fail/off alarms through several interventions, including daily electrode changing, custom alarm parameters, software modification, and clinician education (Cvach et al. 2013; Graham and Cvach 2010). Both studies by Cvach et al. (2013) and Graham et al. (2010) demonstrated an increase in the total number of ECG lead fail alarms by 39 and 314, respectively. In these instances, nurse susceptibility to alarm fatigue and exposure to audible alarms may have been reduced, but arrhythmia detection may also have been impacted. It’s unclear whether this was a significant issue since the time in this alarm condition nor clinical features associated with this alarm condition were reported. Within our dataset, we found that documented cognitive impairment and tremors were associated with ECG lead failure. The mean time within this alarm condition was almost 20 minutes. However, the vast majority of lead fail alarms were between 2 seconds and 5 minutes. These findings offer important evidence that these types of alarms are generated after only a short duration of time in this alarm condition. One solution may be to add a delay for these types of alarms in the configuration setting. However, the optimal delay time needs further investigation to ensure patient safety. In the study by Drew et al. (2014), 90,547 single lead fail alarms (inaudible messages) occurred over a one-month timeframe. It’s important to note that ECG leads fail, which we report, will sound an audible foghorn tone. While their study only provided data for single ECG lead failure, our study showed that 99.4% of ECG lead failure alarms were between 2 seconds and 5 minutes in duration. Some of these are likely to be considered a nuisance and exacerbate the level of noise and possibly alarm fatigue within a busy ICU. In a secondary data analysis of this study in patients with an LVAD, there were 854 ECG lead fail alarms during a one-month time period (Watanakeeree et al. 2021). Even though this study provided valuable insight into a clinical feature that affected technical alarm rates in LVAD patients, generalisability is reduced since only three patients were examined. ECG leads fail alarms can pose an increased risk for alarm fatigue and may compromise patient safety. A randomised study examining the difference in alarm events between disposable and reusable lead wires showed a decrease in the total number of all false alarms (i.e. no telemetry, leads off/fail artefact, and false crisis) when using disposable lead wires (Albert et al. 2015) Non-inferiority statistical analysis also demonstrated that disposable lead wires might be a reasonable approach as a potential solution for reducing technical alarms during continuous ECG monitoring. For each type of technical alarm, the vast majority were found to be between two seconds and 5 minutes (99.2-99.4%). Duration of alarms between 5 minutes and 15 minutes was extremely uncommon (0.1-0.6%), which may suggest that current technical alarm algorithms are too sensitive and should be designed with a delay. As previously discussed, our evidence shows that clinical features (e.g., current smoker, documented tremor, or cognitive impairment, etc.) are associated with higher incidence rates for certain types of technical alarms. Technical alarm thresholds should also be adjusted with the goal of reducing nuisance alarms caused by known clinical features from the patient’s EHR. Several limitations warrant consideration. While we provide new information on the number and types of technical alarms, we did not correlate technical alarms with a patient’s status at the time of the alarm (i.e., bathing, changing electrodes, repositioning, tests at the bedside, etc.). This means the nurse may have been at the bedside with the patient, and the alarm had minimal impact on alarm burden/fatigue. Because only one vendor’s monitor was used, we do not know if our findings are generalisable to other device manufacturers. The study’s retrospective design did not allow us to evaluate how alterations in alarm settings (e.g., turn off, adjust to inaudible setting) would impact the number of alarms identified. Despite these limitations, our study represents the most comprehensive evaluation of technical alarms in a consecutive sample of ICU patients done to date. The vast majority of technical alarms were for artefact. Arrythmia suspend(software off) due to sustained artefact was uncommon.However, the mean time patients were in this technical alarm condition was 10 minutes, which could be important for ICU patients since arrhythmia detection may be compromised. Individual alarms lasted only seconds, which suggests that technical alarms are too sensitive and should be re-designed with a delay (e.g., 5 minutes) before alarming. Patients who were current smokers at admission were more likely to have artefact and arrhythmia suspend alarms. Having a tremor was associated with all three types of technical alarms. Documented cognitive impairment was associated with arrhythmia suspend and ECG leads fail alarms. Patients treated with mechanical ventilation had fewer alarms (all three types). Patients with these features may require more guided alarm management strategies and/or treatment for nicotine withdrawal, or tremor as they are more likely to generate technical alarms. This study was funded by the University of California, San Francisco (UCSF) School of Nursing Lipps Research Fund (Pelter, PI) None. 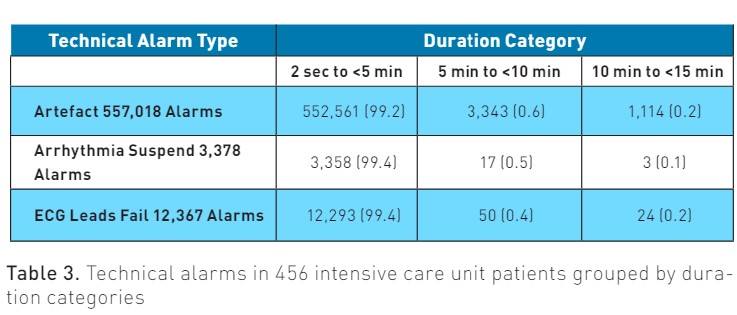
Univariate and Multivariate Analysis
Discussion
Artefact
Arrhythmia Suspend
ECG Leads Fail
Alarm Duration
Limitations
Conclusion
Funding
Conflict of Interest
References:
Albert NM, Murray T, Bena JF et al. (2015) Differences in alarm events between disposable and reusable electrocardiography lead wires. Am J Crit Care. 24(1):67-73; quiz 74.
Bawua LK, Miaskowski C, Suba S et al. (2022) Thoracic Impedance Pneumography-Derived Respiratory Alarms and Associated Patient Characteristics. Am J Crit Care. 31(5):355-365.
Bonafide CP, Lin R, Zander M et al. (2015) Association between exposure to nonactionable physiologic monitor alarms and response time in a children's hospital. J Hosp Med. 10(6):345-51.
Cvach MM, Biggs M, Rothwell KJ, Charles-Hudson C (2013) Daily electrode change and effect on cardiac monitor alarms: an evidence-based practice approach. J Nurs Care Qual. (3):265-71.
Dee SA, Tucciarone J, Plotkin G, Mallilo C (2022) Determining the Impact of an Alarm Management Program on Alarm Fatigue among ICU and Telemetry RNs: An Evidence Based Research Project. SAGE Open Nurs. 8:23779608221098713.
Drew BJ, Ackerman MJ, Funk M et al. (2010) Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 55(9):934-47.
Drew BJ, Harris P, Zègre-Hemsey JK et al. (2014) Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS One. 9(10):e110274.
Graham KC, Cvach M (2010) Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms. Am J Crit Care. (1):28-34; quiz 35.
Harris PR, Zègre-Hemsey JK, Schindler D et al. (2017) Patient characteristics associated with false arrhythmia alarms in intensive care. Ther Clin Risk Manag. 13:499-513.
Jeong S, Cho H, Kim YJ et al. (2021) Drug-induced Parkinsonism: A strong predictor of idiopathic Parkinson's disease. PLoS One. 16(3):e0247354.
Lewandowska K, Weisbrot M, Cieloszyk A et al. (2020) Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment-A Systematic Review. Int J Environ Res Public Health. 17(22):8409.
Pelter MM, Carey MG, Al-Zaiti S et al. (2023) An annotated ventricular tachycardia (VT) alarm database: Toward a uniform standard for optimizing automated VT identification in hospitalized patients. Ann Noninvasive Electrocardiol. 28(4):e13054.
Ruskin KJ, Hueske-Kraus D (2015) Alarm fatigue: impacts on patient safety. Curr Opin Anaesthesiol. 28(6):685-90.
Sendelbach S, Wahl S, Anthony A, Shotts P (2015) Stop the Noise: A Quality Improvement Project to Decrease Electrocardiographic Nuisance Alarms. Crit Care Nurse. 35(4):15-22; quiz 1p following 22.
Shin HW, Chung SJ (2012) Drug-induced parkinsonism. J Clin Neurol. 8(1):15-21.
Shue McGuffin K, Ortiz S (2019) Daily Electrocardiogram Electrode Change and the Effect on Frequency of Nuisance Alarms. Dimens Crit Care Nurs. 38(4):187-191.
Suba S, Sandoval CP, Zègre-Hemsey JK et al. (2019) Contribution of Electrocardiographic Accelerated Ventricular Rhythm Alarms to Alarm Fatigue. Am J Crit Care. 28(3):222-229.
Watanakeeree K, Suba S, Mackin LA et al. (2021) ECG alarms during left ventricular assist device (LVAD) therapy in the ICU. Heart Lung. 50(6):763-769.